Review of Intermittent Catheterization and Current Best Practices

Patients may be concerned almost the discomfort associated with intermittent catheterization(IC), the need to maintain privacy, the fear of performing the catheterization, and the inability to find a make clean and advisable toilet or bathroom for catheterization when traveling exterior their dwelling house. Clinicians need to consider these patient concerns in their teaching and recommend possible strategies.
Teaching Catheterization:
Successful intermittent cocky-catheterization (ISC) requires education and back up, particularly during initial teaching and follow up. Although long term ISC is safe and well accepted, an early dropout rate of virtually xx% has been described in children and adolescents (Pohl et al., 2002), so good support, professional instruction on catheterization technique and periodic follow-up is necessary to obtain and maintain patient compliance. A knowledgeable and experienced clinician, in well-nigh cases a nurse, is an important component for successful self-catheterization teaching. The nurse should assess what the patient and/or the person performing the catheterization knows near the urinary tract and functions of the bladder. Providing an overview of anatomy with pictures or the utilize of an anatomic model of the perineum tin exist very helpful. Many catheter manufacturers have visual guides or videos that tin be used when teaching patients and/or caregivers.
Other pedagogy components include how to handle the catheter, identifying the urinary meatus, and intendance of the catheter. It is of import that patients and/or the person performing the catheterization demonstrate understanding and/or power or perform catheterization nether the supportive supervision of the nurse.
Teaching Surround:
Most adults acquire best under low to moderate stress, so it is important to teach self-catheterization in a depression stress setting. The nurse should also assess the patient'southward power to learn intermittent self-catheterization (ISC), motivation to continue long-term catheterization, awareness of problems associated with catheterization, and the agreement of how to avoid possible complications. Other factors to consider are the patient's bladder capacity (even so voiding some amounts or complete retentiveness), acceptable float outlet resistance (absence of urethral scarring, strictures or enlarged prostate), absence of urethral sensitivity to hurting with catheterization, and patient's possible fearfulness of catheterization. Initially, many patients may be extremely reluctant to perform any procedure that involves the genitals, but this is basically a "fright of the unknown." Determining acceptance of intermittent catheterization is vital considering non-compliance is seen in many patients, particularly adolescents.
General Cess:
Many clinicians are concerned about didactics an older patient ISC but age is non necessarily a determinant to the success of ISC. Disabilities, such equally poor eyesight or blindness, poor hand dexterity, lack of perineal sensation, tremor, mental disability, and paraplegia, exercise not necessarily preclude the ability to perform ISC. But these obstacles may exist hard to overcome in some patients and caregivers. Didactics a patient with a spinal string injury perhaps even more of a challenge because motor and sensory impairment may require changes to catheterization techniques. Impaired cerebral function tin affect success in being able to carry out the procedure independently.
Important Medical History:
Any previous experience with catheterization (e.g indwelling or IC) should be determined prior to education a patient ISC as this will directly the didactics and should be considered when choosing a catheter. In a male patient, a history of urethral strictures or scarring or enlarged prostate may signal need for a Coudé tip catheter. If a adult female has pelvic organ prolapse, angling the catheter effectually the prolapse may exist needed.
Choosing the catheter:With advances in catheter applied science, the number of catheter types and designs has increased, adding complexity to the catheterization process for both the nurse and the patient. Catheter types are now gender specific, long length for males, shorter length for females. acknowledging the anatomical differences in urethral length between men and women.
Blueprint changes include the integration of all needed equipment (such as catheter, water-based
lubricant, and drainage bag) into a compact and user friendly organization. These are referred to equally "airtight systems or kits". Just some patients with limited dexterity may find it difficult to advance a catheter through a collection bag.

When recommending a catheter, consider the patient'southward lifestyle including plans for catheter storage, carrying, and disposal. Offer a option of iii to four types of catheter is recommended.
Catheterization Position:
IC didactics includes identifying the best position for performing catheterization and information technology should be individualized for each patient. Variables to consider when assessing a patient for the ideal position includes abnormally high body mass alphabetize and body hiatus (large pannus) as both could restrict perineal and urethral access. Well-nigh patients tend to catheterize in their bathroom, sitting on or continuing in front of a toilet. For someone who is in a wheelchair most of the mean solar day, catheterizing while sitting in the chair is an choice just maybe more than difficult for women. Women may choose to utilize a mirror to visualize the urethra is also an option.
Catheterization Schedule: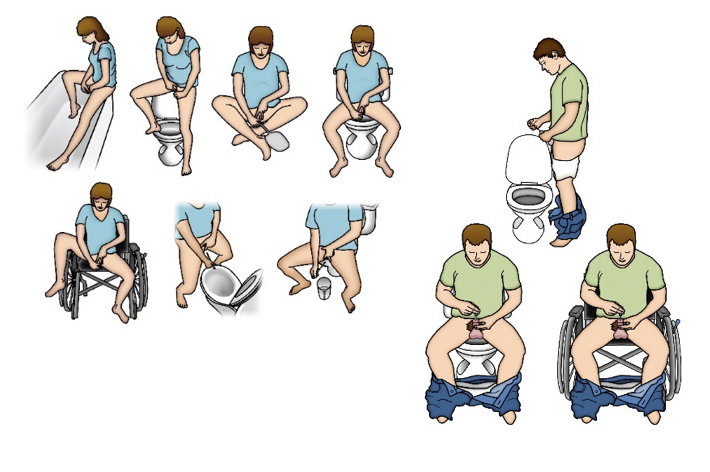
The frequency of catheterization depends on patient history and the clinical reasons for initiating an IC programme: for instance, the individual with reflux and symptomatic UTI will require more frequent catheterizations than the person who is using IC to manage leakage caused by incomplete emptying and who has no UTI symptoms. A catheterization schedule can exist recommended based on frequency-volume records, functional float capacity based on urodynamics findings, ultrasound bladder scans for PVR, and the impact of catheterization on a patient'southward quality of life. As a general rule, bladder book should not exceed 500 mLs, and some abet not exceeding 400 mLs. Based on an private'due south average output, catheterization is usually performed iv to half dozen times during the day. Many patients, especially older patients, may demand to catheterize at bedtime and during the night. The bladder should exist emptied completely with each catheterization. When starting intermittent catheterization, the patient and/or caregiver should record the amount of urine tuckered from the float. If the patient voids, catheterization should always be performed after voiding.
Catheter Use and Care:
As at that place are no clear guidelines almost the length of time for catheter employ if the patient is re-using an uncoated catheter, re-using the same catheter for multiple catheterizations is not recommended. The cleaning of the catheter between uses has no basis in research because there are no published randomized controlled clinical trials of cleaning methods. The comparative effectiveness of cleaning methods, therefore, is unknown.
recommended. The cleaning of the catheter between uses has no basis in research because there are no published randomized controlled clinical trials of cleaning methods. The comparative effectiveness of cleaning methods, therefore, is unknown.
Currently, catheter manufacturers do not provide instructions for catheter re-use or cleaning. So all-time practices practise not support the re-use of unmarried-use catheters at this time.There are no set guidelines for monitoring patients performing ISC, although many urologists advocate regular urine cytology and cystoscopy with random or targeted float biopsies.
In reality, many patients performing intermittent catheterization are lost to urologic follow upward.
March 2021
© 2021 Digital Science Press, Inc. and UroToday.com
hodgeslounctirough88.blogspot.com
Source: https://www.urotoday.com/urinary-catheters-home/intermittent-catheters/description/ic-best-practices-for-management.html
0 Response to "Review of Intermittent Catheterization and Current Best Practices"
Post a Comment